Medical Device Manufacturing Process optimized for Qualitative and Faster Production
A faster and more robust manufacturing process for implantable medical devices
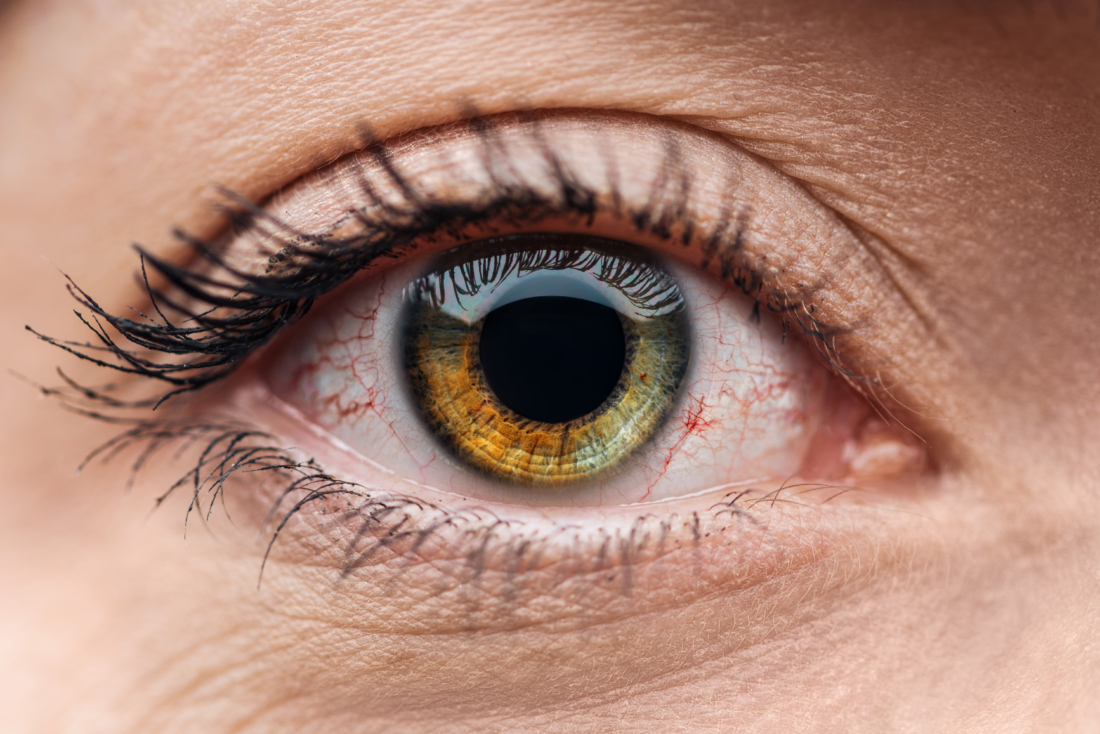
We recently had the privilege of assisting one of our clients, a global medical company dedicated to ophthalmology, in developing and implementing a new, faster, and more robust manufacturing process for their IIb class medical devices.
The client, which operates in over 90 countries and manufactures and distributes medical devices, approached us for a new medical device manufacturing process that would fully address some of their key challenges:
- their current manufacturing processes couldn’t keep up with their growing sales
- they needed a solution that would enable them to meet increasing demand while improving the quality and efficiency of their manufacturing process.
To address these challenges, our team set a few objectives.
Objectives of our client
- First, we aimed to improve the quality of the products, both in terms of their material properties and aesthetic qualities, as well as in terms of repeatability and robustness, which would provide greater confidence in the manufacturing process.
- Second, we wanted to reduce the manufacturing time of the implants, both by improving the process and increasing yields.
- Finally, we needed to coordinate the manufacturing process between two different manufacturing sites in the USA and Belgium, which presented several logistical challenges.
Our approach to implement the new medical device manufacturing process for a Class IIb MD manufacturer
The approach we took to implementing the new manufacturing process was quite general. Nevertheless, it involved all departments and resources, which made it very complex.
We started by deciding which product would be the easiest to begin with, and then added other products to this design change.
R&D department
We worked with the R&D department to ensure that the product specifications remained the same and that equivalence was proven for each User Requirement Specification (URS). URS are very wide and define all the properties of the final product. Most important for an implantable device is that is must be biocompatible and sterile. It must not induce any inflammatory reaction to the customer or any other biological non-desired response. A review of the validation file and an update in the endotoxins testing may be necessary, depending on the impact with the sterilization cycle.
Industrialization
Industrialization for the transposition of the process to a larger scale as well as the integration of new product flows on the existing lines. Reviewing a lot of documentation such as risks analysis (PFMEA) or Device Master Records (DMRs) is necessary. As R&D step, we must ensure that the final product is equivalent to the legacy one, in respect of its specifications and drawings. This includes redaction of protocols and reports for process validation and First Article Inspection with the new process. To match the current process, many tools had to be developed to improve the handling of the device. Furthermore, we also updated the working instructions and trained the operators.
Quality Assurance
Quality assurance was also crucial in this process, as we needed to integrate procedures and audit new critical suppliers. As the process was split between two manufacturing sites, we had to ensure that the QMS from these two entities were compatible. Also, no lack of traceability was allowed. We established a specific Certificate of Analysis (and conformity) to have all the semi-finished product specifications checked at reception prior to pursuing with the process.
Regulatory Affairs
Regulatory Affairs played an important role in the process as well. They were involved both in the very early stages of the change implementation and in the latest stages. The Regulatory Affairs defined the scope of submission and the strategy next to it, such as submitting to Europe first, followed by the USA, and so on. They also gathered feedback from each involved regulatory authority on how critical they evaluated the design change to be. Depending on the answer, we either prepared a submission or a notification. These two scenarios occurred on the latest stage of the change, meaning sending this notification or submission to regulatory authorities. The submission was, basically, all the documentation proving the equivalence of the final product and the absence of risk to the patient. It went along the Design History File (DHF) and detailed all the testing and studies performed.
Coordination
We helped coordinate multiple departments and resources to implement a new manufacturing process for our client’s medical devices. Our approach involved a comprehensive and cross-functional effort that spanned R&D, industrialization, quality assurance, and regulatory affairs.
As part of our coordination efforts, we were responsible for managing tasks and cross-functional tasks. We ensured the update and creation of documentation to prove equivalences, and to build the submission package for the technical file. A yearly budget had to be established: capital expenses (CAPEX including premises, large equipment) and operation expenses (OPEX including samples, tools, testing). We worked to manage suppliers/labs by ordering tests, following up on external testing progress, and ensuring that quotations were paid on time.
Results of this new medical device manufacturing process
Overall, our work helped to achieve significant improvements in the quality and performance of the implantable medical devices.
- With more than 97% of tested implants meeting requirements.
- The process yields increased by more than 30% compared to the previous manufacturing processes.
Our work involved testing for biocompatibility equivalence, which showed results similar to the legacy products. Additionally, we submitted the first product to the notified body dedicated to Europe, and feedback has been encouraging.
Our coordinated efforts played a critical role in helping our client achieve its objectives of:
- improving the quality of its products,
- gaining time on manufacturing,
- and coordinating manufacturing between two sites while meeting international regulatory requirements.
Discover how Alispharm can help you with your current challenges.




